Biopsychosocial Concept Map for Managing Renal Failure in Nursing
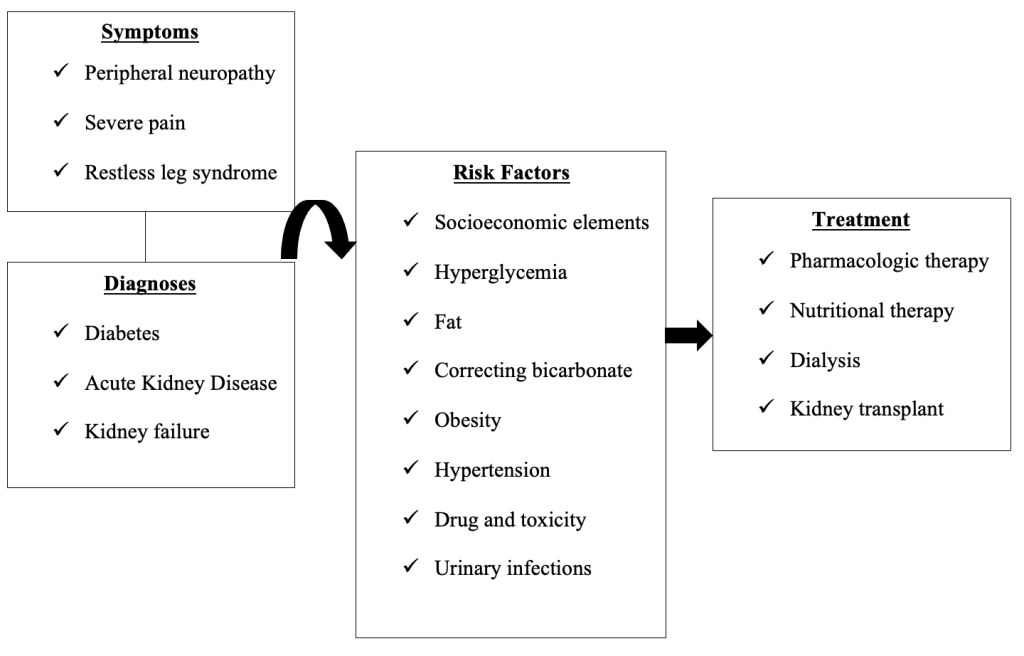
Figure 1: Concept map for managing a patient with renal failure at the acute care facility
Sources:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8268456/
https://www.kidney-international.org/article/S0085-2538(22)00507-5/fulltext
https://doi.org/10.1016/j.kint.2022.06.008
https://www.mayoclinic.org/diseases-conditions/kidney-failure/symptoms-causes/syc-20369048
https://nurseslabs.com/chronic-renal-failure/
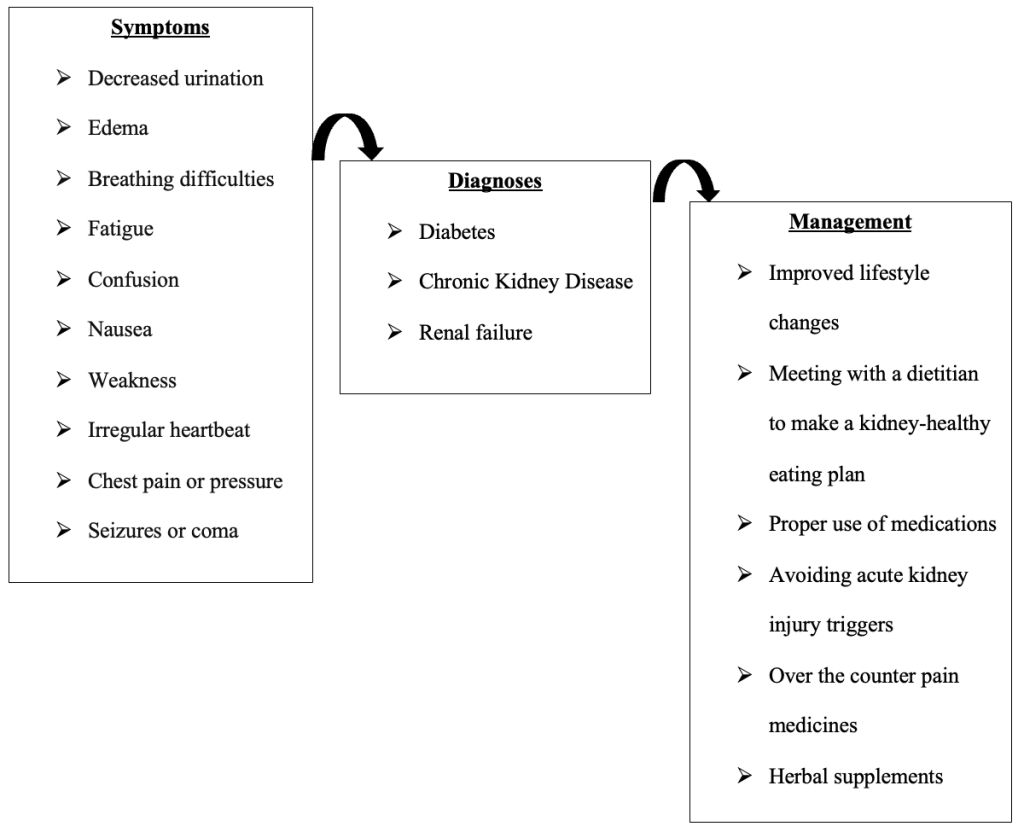
Figure 2: Concept map for managing a patient with renal failure at the health community setting
Sources:
https://www.cdc.gov/diabetes/managing/diabetes-kidney-disease.html
https://www.mayoclinic.org/diseases-conditions/chronic-kidney-disease/symptoms-causes/syc-20354521
Part 2: Additional Evidence
Renal failure can begin as an acute kidney disease (AKD) and progress to become a chronic kidney disease (CKD) depending on the existing management processes. Management at the acute care facility is likely to detect AKD, while management at the community setting is best-suited in handling CDK. ADK is diagnosed when there is a presence of kindly damage markers for about 90 days, whereas the advance kidney disease is confirmed when there is prolonged kidney injury especially for diabetic patients (Buades, et al., 2021). Accordingly, medical tests are necessary for confirmatory diagnoses.
Struggling with a concept map for managing renal failure or other complex nursing assignments? Our team offers expert nursing homework assistance to help you connect pathophysiology, pharmacology, and patient care in a clear, evidence-based way. Get professional support through our nursing assignment help service and simplify even the toughest healthcare projects. Achieve higher grades with tailored guidance designed for nursing students.
Renal disease prevention and management is the most critical process in responding to renal failure associated with diabetes. The final approaches the renal facilities can offer are dialysis and kidney transplant. However, appropriate guidelines must be followed regarding dialysis or transplant methods. Glomerular filtrate rate (GFR) is one of the elements considered during renal failure decision-making. For instance, GFR is highly considered when referring a patient for renal dialysis or transplant. Nonetheless, Buades, et al. (2021) advises that both the symptoms and GFR levels must count for definite decisions concerning the management of a patient with diabetes-related renal failure.
Managing the patient at the community setting can produce excellent results. Buades, et al. (2021) recommends training the healthcare fraternity on the significance of early patient nephrology referral to avert adverse health outcomes. In this case, management ate the community setting is likely to reduces case of kidney failure and mortality. Buades, et al. (2021) also emphasize the relevance of having nephrologists-led inter-professional teams in handling patients with renal failure tied to diabetes. Moreover, it is critical to identify and regulate the risk factors associated with renal failure among diabetic patients. Regardless, combining clinical and community based management of the renal failure among the diabetic patients is the best option.
Multiple health professionals handle patients with renal failure related with diabetes. Even though nursing crew play a central part in helping such patients, other specialists aid in the process. For example, nephrologists, surgeons, endocrinologists, radiologists, physiotherapists, psychologists, and nutritionists, are necessary and Buades, et al. (2021) assert that they must all collaborate for improved positive health outcomes. Both acute and chronic kidney diseases are challenging to detect, diagnose, and management. Accordingly, effective linkage among health experts is paramount.
Health workers both at the hospital and community levels must offer adequate health education regarding kidney issues. For instance, patients must be educated that both kidneys are composed of millions of nephrons, which control the organ’s functions. Training patients on the kidneys’ anatomy and physiology will enable them to appreciate the relationship between kidney problems and other complications as it is the case for renal failure and diabetes. Therefore, patients must be informed that elevated blood sugar levels compromise kidneys’ blood vessels and the filters, which is also the case when diabetes couples with high blood pressure (KDIGO, 2022). Nevertheless, community health workers should educate people on the signs and symptoms of renal diseases, which will then prompt them to proceed to the acute care facility.
Pharmacology and nutritional therapies are essential treatment techniques. Nonsteroidal mineralocorticoid antagonists (MRA) are best suited for patients with increased risk of developing CKD coupled with cardiovascular challenges (Ostermann, et al., 2018). Dietary management is an adoption both at the hospital and community levels. KDIGO diabetes work group (2022) advocates for healthy diets and prevention of type 2 diabetes. Moreover, Center for Disease Control (2021) suggest positive lifestyle transformation aimed at preventing or managing diabetes for healthy kidneys.
References
Buades, J. M., Craver,L., Del Pino, M. D., Prieto-Velasco, M., Ruiz, J. C., Salgueira, M., de Sequera, P., & Vega, N. (2021). Management of kidney failure in patients with diabetes mellitus: What are the best options? Journal of Clinical Medicine, 10(13), 2943. doi: 10.3390/jcm10132943
Center for Disease Control. (2021, May 7). Diabetes and chronic kidney disease. https://www.cdc.gov/diabetes/managing/diabetes-kidney-disease.html
Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. (2022). Clinical practice guideline for diabetes management in chronic kidney disease. Kidney International, 102(5S), S1–S127.
Ostermann, M., Chawla, L. S., Forni, L. G., Kane‐Gill, S. L., Kellum, J. A., Koyner, J., Murray, P. T., Ronco, C., Goldstein, S. L., & ADQI 16 workgroup (2018). Drug management in acute kidney disease – Report of the Acute Disease Quality Initiative XVI meeting. British Journal of Clinical Pharmacology, 84(2), 396–403. doi: 10.1111/bcp.13449